
gynaecological
cancers
Gynaecological cancers have some of the worst outcomes for women, with a devastating mortality rate of 37%. 21 women will die of a gynaecological cancer today and 60 women will be diagnosed.
Understanding the symptoms will save lives, which is why we are calling on you to talk more openly about these life-saving issues.
To jump to a specific type of gynae cancer please use the links below:
Are you looking for our
downloadable resources?
cervical cancer
This is probably the one you are most familiar with! Cervical Cancer can be found anywhere in the cervix. Nearly all cervical cancers are caused by an infection from certain types of human papillomavirus (HPV). It can often be prevented by attending cervical screening and uptake of the HPV vaccine.
Around 3,300 women are diagnosed with cervical cancer in the UK each year, most commonly diagnosed between 30 and 35 years.
-
Around 3,300 women are diagnosed with cervical cancer in the UK each year and it’s the most common cancer in women under 35 years old.
Cervical screening is essential because cervical cancer can be prevented. The NHS cervical screening programme offers testing to women between the ages of 25 and 64. More than four million women are invited for cervical screening each year in England. Around 1 in 100 women screened will have an abnormal result. This does not mean that all women with an abnormal test will develop cervical cancer. Early treatment can prevent these cervical changes from developing into cancer.
-
The most common symptoms of cervical cancer are:
Bleeding from the vagina at times other than when you are having a period
Vaginal discharge that smells unpleasant
Discomfort or pain during sex
If you have any of the symptoms listed above, particularly if:
They are not normal for you
They are persistent
There are repeated episodes
They do not go away
… be sure to visit your doctor for a check up.
Remember, most women with symptoms like these do not have cancer. Your awareness of your symptoms is the first and most important step – early diagnosis can save lives.
-
Human papilloma virus (HPV) is the major cause of cervical cancer.
(Risk factors are characteristics at the biological, psychological, family, community, or cultural level that precede and are associated with a higher likelihood of negative outcomes.)
It is passed on through sexual contact. All children aged 12 or 13 in the UK are routinely offered the HPV vaccine at school. You can get the HPV vaccine for free on the NHS up to your 25th birthday. These vaccines protect against the strains of HPV that are most likely to cause cervical cancer.
Other risk factors include smoking, HIV and taking the pill. Women with a weakened immune system and those who have had a large number of children are also more likely to get cervical cancer.
-
Treatment For Abnormal Cervical Cells -
There are several different treatments available for precancerous changes in the cervix. They all aim to remove or destroy the abnormal cells. This can be done by freezing, with heat from a laser or hot probe, or by cutting out the affected area.
If you are past your menopause or have had all the children you want to have, your doctor may suggest removing the whole of your womb. This is more likely if you have had abnormal cells found on your cervix more than once, or if the abnormality found was severe. In other words, you have not got cervical cancer, but the abnormal cells on your cervix are closer to becoming cancerous cells.
Treatment For Cervical Cancer -
Early cervical cancer can usually be cured with surgery or radiotherapy or both. Surgery usually means that you have your womb and cervix completely removed (hysterectomy). Radiotherapy involves having treatment to the womb, cervix and surrounding tissues. Specialists sometimes suggest radiotherapy after surgery to lower the risk of the cancer coming back. If the disease is still in the very early stages and has not spread to the lymph nodes, surgeons may be able to undertake fertility-sparing surgery (trachelectomy- removal of cervix), for women of childbearing age.
Advanced cervical cancer is usually treated with chemotherapy and radiotherapy together or chemotherapy alone. Even if your cervical cancer cannot be cured there are treatments available to control the symptoms. Specialists will discuss and put together a treatment plan for you.
Click here to find out more from the NHS website.
-
Ovarian cancer can affect women, some transgender men and non-binary people assigned female at birth.
More than 8 out of 10 cases of ovarian cancer occur in women over the age of 50.
-
Women with a very early stage of ovarian cancer often don’t have any symptoms at all. The symptoms may be very vague but can include:
Feeling bloated (having a swollen tummy)
Feeling full quickly and / or loss of appetite
Pain or discomfort in the lower tummy area and / or back
Needing to pass urine more often or more urgently
Changes in bowel habits
Constipation
Weight gain or weight loss
Unexplained or extreme tiredness
If you have any of the symptoms listed above, particularly if:
They are not normal for you
They are persistent
There are repeated episodes
They do not go away
… be sure to visit your doctor for a check up.
Remember, most women with symptoms like these do not have cancer. Your awareness of your symptoms is the first and most important step – early diagnosis can save lives.
-
About nine out of 10 tumours of the ovary are diagnosed as epithelial ovarian cancer.
(Risk factors are characteristics at the biological, psychological, family, community, or cultural level that precede and are associated with a higher likelihood of negative outcomes.)
In these cases, the cancer may have started in the surface layer covering the ovary. Cancers may have started development in the fallopian tube. We don’t know exactly what causes epithelial ovarian cancer, but some factors may increase the risk while other factors seem to reduce it. The risk of ovarian cancer may be increased by the following factors:
01 — Getting Older
As with most cancers, the risk of developing ovarian cancer increases as you get older. Most cases are in women who have had their menopause.
02 — Inherited Faulty Genes
Most ovarian cancers are due to gene changes that develop during a woman’s life and are not inherited. About one to two in 10 ovarian cancers are caused by an inherited faulty gene. Faulty inherited genes (mutations) that increase the risk of ovarian cancer include BRCA1 and BRCA2. These genes also increase the risk of breast cancer. If you have very close relatives who have had ovarian cancer or breast cancer you may be more at risk of developing ovarian cancer than other women. Having relatives with ovarian cancer does not necessarily mean that you have a faulty inherited gene in the family. We also now know that over 4 out of 10 women with ovarian cancer who have a BRCA1 or BRCA2 mutation may not have a family history. Tests can now check for faulty BRCA1 or BRCA2 genes.
03 — Previous Breast Cancer
Breast cancer and ovarian cancer can sometimes be due to the same faulty genes. Women who have had breast cancer have up to double the risk of developing ovarian cancer compared to other women in the population, and if their breast cancer was diagnosed before the age of 40, their risk is around four times higher.
Other factors that can increase the risk are infertility, long-term use of hormone replacement therapy (HRT), being overweight, a diet high in animal fats, and having endometriosis.
-
Most women with a new diagnosis of ovarian cancer are treated with a combination of surgery and chemotherapy.
It is important to be treated at a cancer centre where specialists will discuss and put together a treatment plan for you.
Ovarian cancer
Ovarian cancer is when abnormal cells in the ovary begin to grow in an uncontrolled way. Over 7,500 women are diagnosed with ovarian cancer in the UK each year, making it the 6th most common cause of cancer death in females in the UK.
Click here to find out more from the NHS website.
vaginal cancer
Vaginal cancer is a very rare cancer that's found anywhere in the vagina. It's most common in women aged 75 and over. Anyone with a vagina can get vaginal cancer.
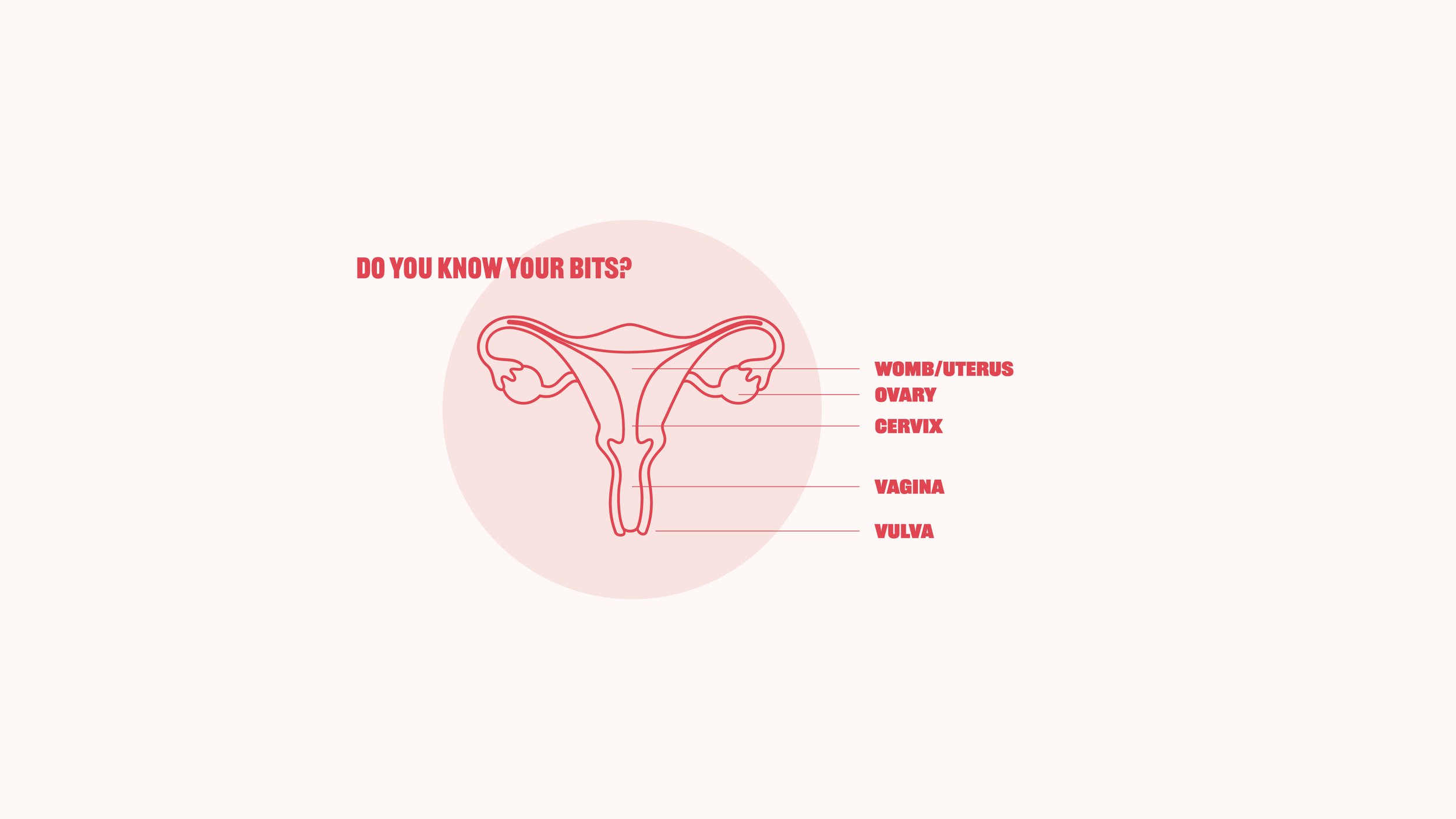
The vagina is a tube between the vulva and the opening of the womb (cervix). Check the anatomy diagram above to see where it’s located!
Vaginal cancer is nearly always caused by an infection from certain types of the human papillomavirus (HPV). It can often be prevented by attending cervical screening and uptake of the HPV vaccine.
-
Vaginal cancer is rare with just under 260 new cases diagnosed in the UK each year. That is less than one out of every 600 cancers diagnosed in women.
-
It’s rare to have symptoms if you have very early vaginal cancer or abnormal cell changes in the lining of the vagina, called vaginal intraepithelial neoplasia (VAIN).
As many as 20 in 100 women (20%) diagnosed with vaginal cancer don’t have symptoms at all. Your doctor may pick up signs of VAIN or very early vaginal cancer during routine cervical screening.
As with most cancers, doctors can successfully treat this early stage of the disease.
The most common symptoms of vaginal cancer are:
bleeding in between periods or after menopause
bleeding after sex
vaginal discharge that smells or is blood stained
pain during sexual intercourse
a lump or growth in the vagina that you or your doctor can feel
a vaginal itch that won’t go away
If you have any of the symptoms listed above, particularly if:
constipation
feeling unable to completely empty your bowels even if there is nothing there to come out
swelling in your legs (oedema)
pain in the pelvic area that won’t go away
pain when going for a wee, blood in your wee, or going more often than usual
… be sure to visit your doctor for a check-up.
Remember, most women with symptoms like these do not have cancer. Your awareness of your symptoms is the first and most important step – early diagnosis can save lives.
-
One of the risk factors is age – as women get older their risk of vaginal cancer increases. More than 70% of cases occur in women aged 60 and over. It is an extremely rare type of cancer in women younger than 40.
A condition called vaginal intraepithelial neoplasia (VAIN) can mean you are more at risk of getting vaginal cancer. It means there are changes to the cells in the inner lining of the vagina. These changes are not enough to make the cells cancerous but they could become cancerous if not treated.
A hormone drug called diethylstilbestrol (DES) is a drug that doctors sometimes gave to pregnant women in the past to stop them from having a miscarriage. DES was only used between 1945 and 1970 and researchers are still gathering information about its effects. The daughters of women who took DES during their pregnancy are more at risk of getting a type of vaginal cancer called clear cell adenocarcinoma, although it’s very rare.
Women who have had genital warts caused by the human papilloma virus (HPV) may have a slightly higher risk of developing vaginal cancer. Women who have had radiotherapy to the pelvic area may also have a very slightly increased risk.
-
There is no screening programme for vaginal cancer because it is a very rare condition.
But when you have a cervical screening test, the doctor or nurse does a routine examination of your vagina at the same time. They can pick up precancerous conditions such as VAIN during this examination. If you have treatment for VAIN, this can prevent vaginal cancer from developing.
The treatment for vaginal cancer depends on a number of factors, including your general health and the stage, grade and type of cancer. Radiotherapy, surgery and chemotherapy may be used to treat vaginal cancer. You may have one, or a combination, of these treatments. Specialists will discuss and put together a treatment plan.
Click here to find out more from the NHS website.
vulvaL cancer
The vulva is a woman's external genitals. It includes:
The lips surrounding the vagina (Labia Minora and Labia Majora)
The Clitoris, the sexual organ that helps women reach sexual climax
The Bartholin's Glands, 2 small glands on each side of the vagina
Most of those affected by vulval cancer are older women over the age of 65.
The condition is rare in women under 50 who have not yet gone through menopause.
-
Vulval cancer is a rare cancer. Around 1,200 cases are diagnosed in the UK each year. It is more common in older women and many cases are diagnosed in women aged 65 or over.
-
Symptoms of vulval cancer can include:
A lasting itch, pain or soreness and thickened, raised, red, white or dark patches on the skin of the vulva.
Open sore or growth visible on the skin
Burning pain when you pass urine
Vaginal discharge or bleeding
A mole on the vulva that changes shape or colour
Lump or swelling in the vulva
If you have any of the symptoms listed above, particularly if:
They are not normal for you
They are persistent
There are repeated episodes
They do not go away
… be sure to visit your doctor for a check-up.
Remember, most women with symptoms like these do not have cancer. Your awareness of your symptoms is the first and most important step – early diagnosis can save lives.
-
The risk of developing vulval cancer increases with age.
Human papilloma virus (HPV) is thought to be responsible for 4 out of 10 vulval cancers. Most women who have HPV infection do not go on to develop vulval cancer. Vulval intraepithelial neoplasia (VIN) means there are precancerous changes in the skin of the vulva. In some women, VIN develops into vulval cancer. The most common symptom of VIN is a lasting itch that does not get better or go away.
Other risk factors include a weakened immune system, genital herpes infection, smoking and some chronic skin conditions.
-
The main treatments used for vulval cancer are surgery, radiotherapy and sometimes chemotherapy.
Your specialist may suggest a combination of treatments.
Click here to find out more from the NHS website.
Womb (Uterus) cancer
Womb cancer is cancer that affects the womb (uterus). It's most common in women who've been through menopause. Anyone with a womb can get womb cancer.
Most womb cancer usually starts in the lining of the womb (endometrium), this is also known as endometrial cancer.
Womb cancer is the fourth most common cancer in women in the UK.
-
Womb cancer is the fourth most common cancer in women in the UK.
About 9,700 women are diagnosed with womb cancer in the UK each year, with around five out of every 100 cancers diagnosed in women being womb cancers. By far the most common type of womb cancer is endometrial cancer. Endometrial means that the cancer starts in the lining of the womb.
-
The most common symptom of womb cancer is:
Abnormal bleeding from the vagina – especially in women who have had their menopause and stopped having periods.
About 90 out of 100 cases of womb cancer are picked up because of post-menopausal or irregular vaginal bleeding. Irregular bleeding can be vaginal bleeding after menopause, bleeding that is unusually heavy or happens between periods or vaginal discharge – from pink and watery to dark and foul smelling.
Less common symptoms can include:
Pain or discomfort in the lower abdomen
Pain during sex
Your womb is enlarged and feels swollen although this will be something which your doctor will be able to see
Advanced womb cancer can cause more symptoms, especially if the cancer has spread to other parts of the body. These are less common and can include:
Loss of appetite and weight
Tiredness or weakness
Feeling or being sick
Constipation
Feeling breathless
Passing urine more often than usual
If you have any of the symptoms listed above, particularly if:
They are not normal for you
They are persistent
There are repeated episodes
They do not go away
… be sure to visit your doctor for a check-up.
Remember, most women with symptoms like these do not have cancer. Your awareness of your symptoms is the first and most important step – early diagnosis can save lives.
-
Womb (endometrial) cancer is most often diagnosed in women aged between 60 and 79.
Over a 1/3 of womb cancers in the UK are linked to lifestyle factors.
Most endometrial cancers are driven by the female hormone, oestrogen. Overweight or obese women are more likely to develop endometrial cancer than women of a normal weight. Factors related to your menstrual history can increase the risk of womb cancer, such as starting periods early or having a late menopause. Having oestrogen-only Hormone Replacement Therapy (HRT) or taking Tamoxifen can also increase the risk of womb cancer. Women with diabetes are more likely to develop endometrial cancer.
You are at a slightly increased risk of getting womb cancer if you have had cancer of the colon, rectum or breast in the past. Similarly, once you have had womb cancer, you have a slightly increased risk of developing certain other cancers. Having a baby lowers your risk of womb cancer and having more than one child lowers the risk even further.
-
Surgery is the first and most important treatment for almost all women with womb cancer.
For some women, this may be the only treatment they need to cure the cancer. Depending on the type of womb cancer you have, your doctor may recommend radiotherapy, hormone therapy or chemotherapy. Specialists will discuss and put together a treatment plan for you.
Click here to find out more from the NHS website.

takeaway Resources
We’ve made some resources that we think could be useful to our community. Share these with your loved ones, or paste them around town. We’ll let you decide how you think is best to get the most people talking.
the vagina dialogues
Let’s not beat around the bush. It’s why we’ve fanny packed this little guide with lots of learning about those lovely bits between your legs.
5 gynae cancer factsheets
Like most cancers, the earlier you spot and treat gynae cancers, the more treatable they are - so we’ve put together some factsheets for you.
signs & symptoms poster
Did you know? 78% of British women are unaware that there are in fact five gynaecological cancers - read all about them here.
symptom tracker
Awareness of the symptoms is low, and often they can be hard to recognise - it’s what makes paying attention and knowing your body’s normal so important.
BLOOM acronym poster
BLOOM is an acronym to remember to check for any gynaecological concerns! It includes a summary of the most common symptoms of the five gynaecological cancers.